by Dr Gene | May 15, 2025 | Health
Every day, millions of Americans turn on their faucets and fill glasses with tap water, trusting that what flows from the spout is clean, safe, and healthful. Water is, after all, fundamental to life. It composes more than half the human body, and no living organism can survive without it. From hydration and nutrient transport to temperature regulation and detoxification, water plays an essential role in virtually every function of the human body. So it is only natural that we would place tremendous trust in the quality and safety of our drinking water. But what if that trust has been misplaced?
Across the United States, tap water often carries with it a hidden cocktail of contaminants. Though these chemicals are often present in concentrations that comply with federal safety standards, recent research suggests that these standards may be dangerously outdated. For decades, regulatory frameworks have addressed contaminants one by one, a process that is both slow and ill-suited to keeping up with the rapidly evolving landscape of chemical exposure. Meanwhile, new contaminants are discovered regularly, and the long-term health impacts of their combinations remain largely unknown.
Organizations like the Environmental Working Group (EWG) have taken up the mantle of uncovering the truths about the quality of America’s drinking water. Through pioneering research and relentless advocacy, they are shedding light on a harsh reality: even when water meets the current federal legal limits, it may still pose significant risks to public health. Their findings are stark, and they demand a reckoning with the assumptions that have shaped water safety regulations for decades.
One of EWG’s most influential contributions to public knowledge is their Tap Water Database. It is a sweeping repository of over 32 million water quality test results from more than 50,000 community water systems across the country. The data paints a troubling picture. Contaminants such as arsenic, radioactive elements like uranium and radium, disinfection byproducts, and nitrate are found in tap water systems serving communities both large and small. While these substances may be individually regulated, their combined effects are often ignored, and science has yet to fully understand the risks posed by these chemical mixtures.
Consider the state of California, where a case study applied EWG’s novel cumulative risk framework to existing water data. Although the water generally met federal safety standards, researchers identified over 20 carcinogens present at levels significant enough to increase the risk of cancer. Their estimates attributed more than 15,000 lifetime cancer cases to drinking water exposure alone. This analysis, published in the journal Environmental Health in 2019, was the first of its kind and challenged the deeply rooted notion that compliance with federal regulations equates to safety.
EWG extended this research to a national scale and found an even more unsettling figure: more than 100,000 additional cancer cases across the United States could be linked to contaminants in tap water. The primary culprits? Arsenic, disinfection byproducts, and radioactive contaminants, especially in communities served by smaller water systems that often rely on untreated or minimally treated groundwater. These smaller systems, due to their limited resources and infrastructure, frequently face higher exposure levels, making them especially vulnerable.
The role of disinfection by products is particularly paradoxical. Chlorine and similar agents are necessary to eliminate bacteria and viruses in water. Without them, communities would be at risk of devastating waterborne diseases. However, when these disinfectants react with organic matter in the water—such as plant debris and sediments—they form toxic byproducts. These compounds, found in the drinking water of most Americans, have been linked to cancer and other health issues, turning a protective measure into a potential hazard.
In 2020, the EWG expanded its testing to include previously unregulated haloacetic acids, a class of disinfection byproducts that had not been thoroughly studied. The results revealed a widespread presence of these chemicals and raised new alarms about the health risks they pose. The data emphasized a critical flaw in how drinking water standards are established: many guidelines are based on outdated science, and they fail to account for real-world exposures to multiple contaminants. To truly safeguard public health, the process must incorporate findings from human studies and reflect the full spectrum of pollutants found in today’s water systems.
Another area of concern is nitrate, a contaminant primarily associated with agricultural runoff. The EPA’s current legal limit for nitrate is aimed at preventing methemoglobinemia, or “blue baby syndrome,” a potentially fatal condition in infants. Yet new research shows that nitrate exposure can also elevate the risk of cancer and harm fetal development. EWG’s 2019 analysis estimated that nitrate pollution in drinking water could be responsible for nearly 12,600 excess cancer cases per year and more than $1.5 billion in health care costs. It may also contribute to thousands of cases of very low birth weight and preterm births annually.
The recommended nitrate limit proposed by EWG is almost 100 times stricter than the EPA’s current standard. This discrepancy underscores the urgent need for updated, health-based guidelines that reflect contemporary scientific understanding. The current federal thresholds, shaped more by political compromise than public health science, are no longer sufficient to protect a nation facing new and mounting environmental challenges.
The broader implication of EWG’s research is that our approach to regulating water safety must evolve. It is no longer enough to assess one chemical at a time, ignoring the synergistic effects that occur when multiple pollutants are present. Instead, we must develop comprehensive frameworks that evaluate the cumulative impact of contaminants. This approach would not only provide a more accurate picture of risk but also better inform decisions about where to invest in water infrastructure and treatment technologies.
Communities served by smaller water systems, particularly those in rural or underserved areas, often face the greatest risks. These systems struggle with limited funding and outdated infrastructure, which hampers their ability to address contamination effectively. Investments aimed at improving water quality must prioritize flexibility and scalability to ensure that even the smallest communities receive the protection they deserve. The stakes are too high to continue leaving these areas behind.
Federal agencies like the EPA are responsible for setting the standards that determine whether drinking water is safe. But as EWG’s findings demonstrate, many of these standards fail to account for the true risks posed by modern-day water contaminants. While a glass of water from the tap may appear clean, its invisible contents could harbor substances that slowly erode health over time. For the average person, the realization that their water may not be as pure as it seems is deeply unsettling. Yet awareness is the first step toward change.
The solution requires a collective effort. Scientists must continue to conduct rigorous research to understand the health impacts of contaminant mixtures. Policymakers must be willing to update outdated regulations and adopt health-protective standards informed by the latest evidence. Communities must be empowered with transparent information about their water supply, and consumers must demand accountability from both industry and government. Change is possible, but it begins with a fundamental shift in how we think about water safety. Drinking water is not just a basic necessity; it is a cornerstone of public health. When the integrity of that foundation is compromised, the consequences ripple through every facet of life. It is time to treat water quality with the seriousness it deserves, to recognize that what we do not see can still harm us, and to work toward a future where every sip from the tap is not only refreshing, but truly safe. That future depends on new frameworks, renewed commitment, and the recognition that the health of our water is inseparable from the health of our people.
by Dr Gene | May 6, 2025 | Health
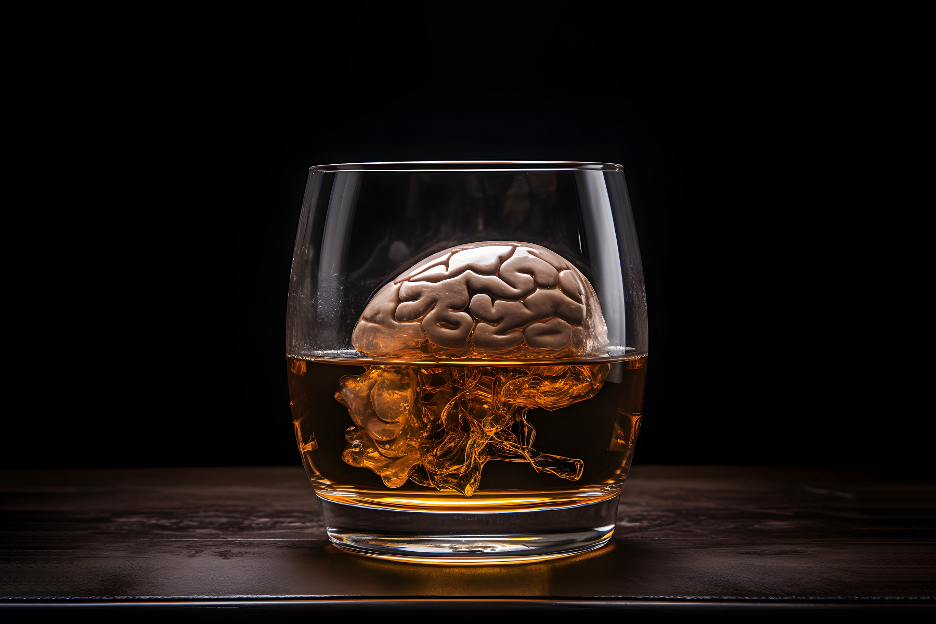
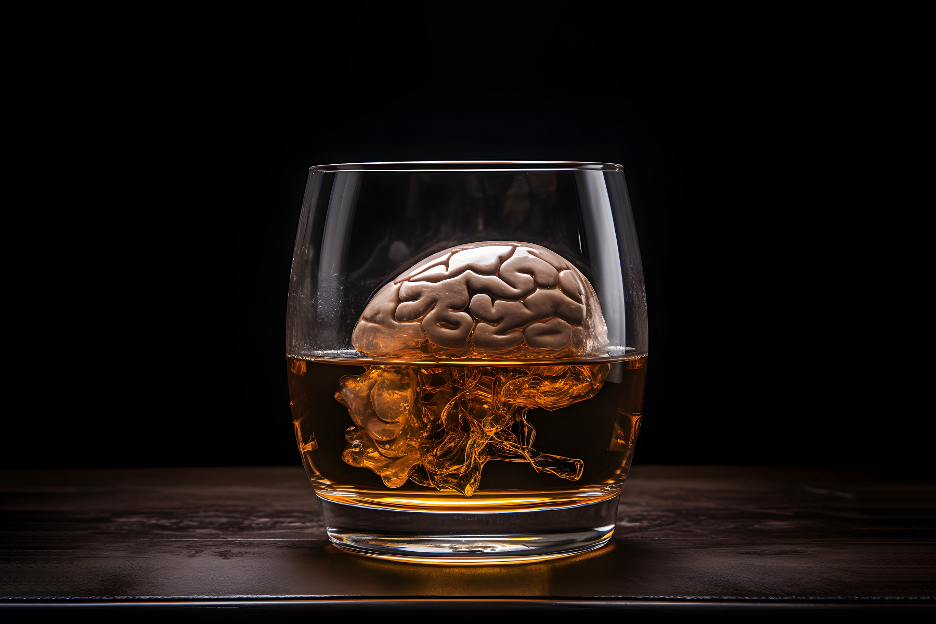
Alcohol is so deeply embedded in modern life that its risks often fade into the background. We toast with it at celebrations, use it to unwind after long days, and sometimes lean on it to soothe our emotions. While occasional, moderate drinking might not seem alarming, chronic and excessive alcohol use can profoundly rewire the brain, making it harder to think clearly, adapt to change, and break unhealthy patterns.
This isn’t just about liver damage or hangovers. The long-term cognitive, neurological, and physiological impacts of Alcohol Use Disorder (AUD) are extensive—and often irreversible. Chronic alcohol consumption alters the architecture of the brain itself, especially in areas involved in memory, decision-making, and behavioral flexibility. It increases the risk of not only liver disease but also stroke, heart disease, and multiple forms of cancer. But perhaps more insidiously, it fundamentally disrupts the brain’s capacity to evolve and learn, trapping individuals in destructive loops.
In this article, we’ll explore how chronic alcohol use reshapes the brain, impairs cognitive flexibility, and creates a feedback loop that makes change even more difficult. We’ll also take a closer look at cutting-edge research, including a recent study out of Texas A&M University, that reveals just how deep these changes go.
The Brain’s Architecture: A Dynamic System
Our brains are remarkably adaptable. The concept of neuroplasticity refers to the brain’s ability to change its structure and function in response to learning, environment, and experience. This plasticity is what allows us to form habits, unlearn them, and build new behavioral patterns. At the heart of this adaptability is the prefrontal cortex, the region responsible for decision-making, planning, and impulse control.
Cognitive flexibility—the ability to adapt our thinking and behavior in response to changing goals or environments—is a crucial function of a healthy brain. It enables us to shift gears, consider alternative perspectives, and break free from rigid behavior patterns. However, when alcohol is consumed regularly and excessively, this plasticity starts to break down.
How Alcohol Hijacks the Brain’s Reward System
Alcohol’s initial appeal lies in its effect on the brain’s reward system. Drinking causes a surge in dopamine, the “feel-good” neurotransmitter that creates sensations of pleasure and relaxation. Over time, the brain becomes conditioned to seek out alcohol as a primary source of reward. This begins to shift brain chemistry and structure in subtle but powerful ways.
With prolonged use, alcohol diminishes natural dopamine production and impairs the function of the very circuits that help us experience reward from healthy activities like exercise, social bonding, or achieving goals. This can lead to emotional numbing, depression, and an inability to find pleasure in previously enjoyable activities—a condition known as anhedonia.
The brain starts to prioritize alcohol above all else, even as the reward from it decreases. This is part of what makes addiction so powerful and so difficult to overcome.
The Role of Cholinergic Neurons and Cognitive Flexibility
A groundbreaking study from Texas A&M University, published in 2023, helps illuminate exactly how alcohol affects the brain at a cellular level. Researchers discovered that chronic alcohol exposure impairs the activity of cholinergic neurons in the basal forebrain—cells critical for cognition and behavioral flexibility.
These cholinergic neurons regulate the release of acetylcholine, a neurotransmitter essential for attention, learning, and memory. They also influence dopamine circuits involved in reward processing. When alcohol interferes with these neurons, it compromises the brain’s ability to switch between tasks and process new information—two essential aspects of learning and adapting to change.
Lead researcher Dr. Jun Wang noted that individuals with Alcohol Use Disorder (AUD) “are less flexible cognitively” and “may not be able to change their behavior even when they are aware of the negative consequences.” This helps explain why many individuals with AUD continue to drink despite knowing the health risks and personal damage. Their brains are, quite literally, stuck in a loop—unable to break free from the pattern even when they want to.
Breaking Habits Becomes Biologically Harder
Habits, by definition, are automated behaviors that our brains develop to save energy and streamline decision-making. Under normal conditions, we can adjust or break habits when they no longer serve us. But with chronic alcohol use, those neural pathways become more deeply entrenched and less flexible.
The impairment of cholinergic signaling and the disruption of prefrontal cortex activity combine to make behavioral change extraordinarily difficult. It’s not simply a matter of willpower; the architecture of the brain no longer supports the process of change.
This is compounded by alcohol’s effect on the hippocampus, the region associated with memory and learning. Chronic drinking can shrink the hippocampus, impair memory formation, and reduce the ability to retain new information—making the learning required to change one’s behavior even harder.
The Physical Toll: Beyond the Brain
While the neurological consequences of alcohol use are devastating in their own right, the physical toll on the body is equally alarming.
Alcohol Use Disorder significantly increases the risk of stroke. Heavy drinking can lead to high blood pressure, irregular heartbeat (atrial fibrillation), and increased clotting—factors that raise the likelihood of both ischemic and hemorrhagic strokes. The American Heart Association warns that drinking more than moderate amounts of alcohol raises stroke risk considerably, particularly when drinking occurs in binge patterns.
Heart disease is another major consequence. Chronic alcohol consumption weakens the heart muscle (alcoholic cardiomyopathy), disrupts rhythm, and raises blood pressure—conditions that can culminate in heart failure or cardiac arrest.
The link between alcohol and cancer is also well-established. The National Cancer Institute lists alcohol as a known carcinogen. It increases the risk of cancers of the mouth, throat, esophagus, liver, breast, and colon. Acetaldehyde, a byproduct of alcohol metabolism, can damage DNA and inhibit the body’s ability to repair damaged cells—key pathways in the development of cancer.
These conditions don’t occur in isolation. Often, the cognitive impairments caused by alcohol hinder an individual’s ability to seek care, follow treatment protocols, or even recognize that a problem exists. Thus, physical and mental health deteriorate in parallel, reinforcing a cycle that becomes harder and harder to escape.
Emotional Regulation and Stress Response
Alcohol’s effect on the amygdala—the brain’s emotion and fear center—further complicates recovery. Chronic use blunts the body’s natural stress response, while at the same time making individuals more sensitive to stress in the absence of alcohol. This creates a paradox: people drink to relax or calm down, but the more they drink over time, the more stressed and emotionally volatile they become when sober.
This dysregulation is one reason why anxiety and depression often go hand-in-hand with Alcohol Use Disorder. Many individuals with co-occurring mental health conditions initially turn to alcohol as a form of self-medication. But instead of offering relief, alcohol ultimately worsens these conditions.
Reclaiming Brain Health: Is Recovery Possible?
There’s good news, though: the brain, while vulnerable, is also resilient. With sustained sobriety and therapeutic intervention, some of the damage caused by chronic alcohol use can be reversed or improved.
Neuroplasticity doesn’t disappear entirely. In fact, after prolonged abstinence, the brain begins to forge new neural pathways, strengthen executive function, and rebuild damaged areas—particularly in the prefrontal cortex and hippocampus. Cognitive behavioral therapy (CBT), mindfulness-based interventions, and exercise can accelerate this process, helping individuals regain control over their thoughts and actions.
Nutritional support is also critical. Chronic alcohol use depletes essential nutrients like B vitamins, magnesium, and omega-3 fatty acids, which are vital for brain health and neurotransmitter production. Supplementation and a diet rich in whole foods, antioxidants, and healthy fats can help support the healing process.
Most importantly, successful recovery often requires a holistic approach—addressing not just the behavior of drinking, but the underlying causes, whether psychological, social, or spiritual. Community, support, and purpose are essential for maintaining long-term sobriety and brain health.
Final Thoughts: Alcohol’s Invisible Toll
Alcohol doesn’t just change the way we feel. It changes who we are, how we think, and what we’re capable of becoming. It rewires our brains in ways that trap us in destructive cycles, making it harder to see clearly, think critically, or make lasting change.
The myths surrounding alcohol—its glamorization, its normalization, and its minimization—have hidden its true costs from view. But research like the Texas A&M study brings new clarity to the conversation. We now know that chronic alcohol use interferes with the very neurons responsible for adapting to life’s challenges. It undermines the systems we rely on to evolve, grow, and thrive.
If you or someone you love is struggling with alcohol use, understanding the neurological reality can foster compassion—and urgency. This is not a failure of willpower. It’s a hijacked brain crying out for help.
Recovery is not only possible—it’s transformative. And with the right support, tools, and knowledge, the brain can heal, learn, and adapt again.
References:
- Wang, J., et al. (2023). Chronic Alcohol Disrupts Cholinergic Neurons in the Basal Forebrain and Impairs Cognitive Flexibility. Texas A&M University. [Published study on cholinergic neurons and alcohol-induced cognitive impairment.]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). (2022). Alcohol’s Effects on the Brain.
- American Heart Association. (2021). Alcohol and Heart Health.
- National Cancer Institute. (2023). Alcohol and Cancer Risk.
- World Health Organization. (2018). Global Status Report on Alcohol and Health.
- Koob, G. F., & Le Moal, M. (2008). Addiction and the Brain Antireward System. Annual Review of Psychology.

by Dr Gene | Apr 18, 2025 | Health
It begins with a simple bite—a crunchy chip, a sip of soda, a warm slice of fast-food pizza. The flavors are bold, almost intoxicating, designed to make you crave just one more. Before you know it, you’ve finished the whole bag, downed the entire drink, or reached for another serving. It feels satisfying, yet strangely, the hunger never quite goes away. If anything, it grows stronger.
This isn’t an accident. The foods that fill supermarket shelves, the ones promoted in bright, colorful packaging, and the meals that promise quick preparation and irresistible flavors are not merely convenient. They are engineered—meticulously designed in food laboratories, with finishing touches by marketing agencies – all with one goal in mind: to keep you coming back for more.
Ultra-processed foods have become the cornerstone of the modern diet. These are not just ordinary processed items like fresh bread, yogurt, or frozen vegetables. No, these are industrial products that are broken down into their most basic components—sugars, fats, and starches—then reconstituted with artificial flavors, preservatives, emulsifiers, and colors to create something that barely resembles real food. The result is a substance so hyper-palatable that it overrides the body’s natural hunger and satiety signals, making it nearly impossible to stop eating.
The chemicals lurking in ultra-processed foods are as varied as they are concerning. Emulsifiers, such as soy lecithin and carrageenan, keep ingredients from separating, giving products their smooth, uniform texture. Artificial sweeteners like aspartame and sucralose add sweetness without calories, yet they disrupt the gut microbiome and leave the body craving more sugar. Preservatives like sodium benzoate and nitrates extend shelf life but have been linked to inflammatory diseases and even cancer. Then there are the flavor enhancers—monosodium glutamate (MSG), disodium inosinate, and others—scientifically crafted to trigger a pleasure response in the brain, making foods more addictive.
Each of these ingredients serves a purpose, not for health, but for profit. They ensure that processed foods last longer, taste more intense, and cost less to produce, all while keeping consumers hooked. And the consequences of consuming these foods regularly are staggering.
The link between ultra-processed foods and obesity is well-established. People who eat diets high in these artificial foods tend to consume far more calories than those who eat whole, natural foods. This isn’t just about portion sizes—it’s about how these foods alter metabolism. With every sip of a sugary drink or bite of a chemically enhanced snack, blood sugar levels spike dramatically, leading to a rapid burst of energy. But just as quickly, they crash, leaving the body desperate for another hit. The cycle repeats, driving overconsumption and weight gain.
But the effects go beyond the waistline. The gut, often called the “second brain,” is particularly vulnerable to the chemicals found in ultra-processed foods. The emulsifiers designed to create a smooth texture in food also disrupt the protective lining of the intestines, leading to conditions like leaky gut syndrome and irritable bowel syndrome. Artificial sweeteners, marketed as healthier alternatives to sugar, interfere with gut bacteria, increasing the risk of metabolic disorders and even affecting mood and cognition. The gut and brain are deeply connected, meaning what we eat influences not just our digestion, but our mental health as well.
Then there are allergies and autoimmune disorders, conditions that have surged in recent decades. More children than ever suffer from food intolerances, eczema, and asthma, and many researchers believe that ultra-processed foods are playing a role. Additives like artificial colors and preservatives can trigger inflammatory responses in the body, making the immune system hyperactive. Red 40 and Yellow 5, two of the most common food dyes, have been linked to hyperactivity in children, while certain preservatives have been associated with increased allergic reactions.
Perhaps the most insidious aspect of ultra-processed foods is their addictive nature, a problem that often begins in childhood. From the moment a toddler is given a sugary yogurt or a brightly colored fruit snack, their taste buds are being trained. Natural flavors, the subtle sweetness of ripe fruit, and the earthiness of vegetables become dull in comparison to the chemically enhanced versions found in processed foods. A child raised on these products often rejects real, whole foods, finding them bland and unappealing.
Food manufacturers understand this. They aim at children using cartoons, catchy jingles, and packaging designed to make their products irresistible. By the time kids become adults, their brains are conditioned to crave these artificial foods. It’s no surprise that so many face struggles with food addiction, finding it hard to resist the allure of fast food, soda, and snacks that have been expertly designed to bypass self-control.
Breaking free from the grip of ultra-processed foods is not easy. The cravings they induce are real, and the body becomes accustomed to the sugar highs, the salt hits, the artificial flavors that trick the brain into thinking it’s receiving nourishment when it’s actually being deprived. But awareness is the first step.
Understanding what’s in these foods, how they manipulate taste and hunger, and what they do to the body can empower people to make better choices. The solution is not about banning all convenience foods but about choosing wisely—favoring whole, minimally processed options, cooking more at home, and retraining the palate to appreciate real flavors.
Children, especially, need to be protected. Instead of reaching for sugary cereals and flavored snacks, they should be introduced to real foods early in life. Parents who cook at home, involve their kids in meal preparation, and create a positive food environment can help break the cycle before it begins.
Ultra-processed foods are not just a dietary issue; they are a public health crisis. The rise in obesity, diabetes, digestive disorders, and even mental health conditions can all be traced back to what we eat. And while food corporations may not have our best interests at heart, we still have a choice.
The next time you reach for a packaged snack, a frozen meal, or a bottle of soda, take a moment to think. Is this food nourishing my body? Or is it just another chemical concoction, designed to keep me coming back for more? The answer might be the first step toward real health.

by Dr Gene | Apr 15, 2025 | Health
In our modern world, pesticides have become an essential part of conventional agriculture, ensuring that crops are shielded from pests, fungi, and weeds. While these chemicals support food production, they also present considerable health risks that are often neglected. Beneath the allure of fresh produce lies a hidden threat—one that can have significant effects on our health.
Many non-organic fruits and vegetables contain high levels of pesticides, some of which are recognized as endocrine disruptors, carcinogens, and neurotoxins. These chemicals can interfere with hormonal balance, hinder metabolism, and contribute to chronic diseases such as obesity, diabetes, and even cancer. A significant concern is the prevalent use of fungicides and insecticides, which can negatively affect human health in ways we are only beginning to comprehend.
Pesticides are substances designed to kill or repel pests that threaten crops. These include herbicides (for weeds), insecticides (for insects), and fungicides (for fungi). While they effectively increase agricultural yields, they also leave behind chemical residues on produce that can be ingested and absorbed into the human body.
Each year, the Environmental Working Group (EWG) publishes its Shopper’s Guide to Pesticides in Produce, identifying the Dirty Dozen—the twelve most contaminated fruits and vegetables—and the Clean Fifteen, which contain the least pesticide residues. In 2024, they analyzed 47,510 samples of 46 different types of produce, revealing shocking results.
Their findings showed that 75% of all conventional fresh produce contained residues of potentially harmful pesticides. For items on the Dirty Dozen list, an astonishing 95% of samples contained pesticide residues. Even after washing and peeling, traces of 254 different pesticides were detected across all tested fruits and vegetables, including 209 different pesticides on Dirty Dozen produce.
Among these contaminants, fungicides such as fludioxonil, pyraclostrobin, boscalid, and pyrimethanil are of particular concern due to their potential endocrine-disrupting properties. These chemicals, used to prevent fungal infections in crops, may interfere with hormonal function, impacting reproductive health and increasing cancer risks.
Fungicides: A Silent Threat to Health
Fungicides are commonly used in conventional agriculture to prevent spoilage, ensuring that produce looks fresh and unblemished. However, research suggests that these chemicals may have unintended consequences for human health.
1. Fludioxonil
Fludioxonil is frequently found on 90% of peaches and nearly 30% of Dirty Dozen samples. Studies indicate that it can mimic estrogen, potentially increasing the proliferation of breast cancer cells. It may also harm the male reproductive system, affecting sperm quality and hormone levels.
2. Pyrimethanil
This fungicide, detected on 54% of pear samples, has been linked to thyroid disruption and hormone interference. Research suggests it may block androgen receptors, impacting testosterone levels and reproductive function.
3. Pyraclostrobin
Found in 10% or more of each Dirty Dozen item and 50% of strawberry and cherry samples, pyraclostrobin is associated with liver toxicity and metabolic disorders. Long-term exposure may contribute to insulin resistance and obesity.
4. Boscalid
This chemical, detected on nearly half of all blueberry samples and over 50% of cherries and strawberries, has been linked to cancer and thyroid dysfunction. Studies suggest it may also disrupt hormone function, leading to developmental and reproductive issues.
The Dirty Dozen: Foods to Watch Out For
According to EWG’s 2024 report, the following 12 items had the highest pesticide contamination levels:
- Strawberries
- Spinach
- Kale, collard, and mustard greens
- Grapes
- Peaches
- Pears
- Nectarines
- Apples
- Bell and hot peppers
- Cherries
- Blueberries
- Green beans
Over 90% of samples from strawberries, apples, cherries, spinach, nectarines, and grapes contained residues of two or more pesticides. Kale, collard, and mustard greens had the highest number of different pesticides, with 103 individual chemicals detected.
The Clean Fifteen: Safer Alternatives
On the other hand, the Clean Fifteen list includes produce with the least pesticide residues. These fruits and vegetables are safer options, whether purchased organic or conventional:
- Avocados
- Sweet corn
- Pineapple
- Onions
- Papaya
- Sweet peas (frozen)
- Asparagus
- Honeydew melon
- Kiwi
- Cabbage
- Watermelon
- Mushrooms
- Mangoes
- Sweet potatoes
- Carrots
Nearly 65% of these items had no detectable pesticide residues, with avocados and sweet corn ranking as the cleanest options.
One of the greatest concerns surrounding pesticide exposure is its impact on children. The American Academy of Pediatrics has warned that exposure to pesticides, even in small amounts, can harm developing brains, leading to cognitive impairments, behavioral disorders, and hormonal imbalances.
A recent study published in Environmental Health found that the EPA has failed to protect children from many pesticides, neglecting to apply legally required safety factors for nearly 90% of the most common pesticides. These findings raise serious concerns about regulatory oversight and the safety of our food supply.
While the dangers of pesticides in food are alarming, there are steps consumers can take to minimize their exposure:
- Choose organic when possible, especially for items on the Dirty Dozen list.
- Wash produce thoroughly to remove surface pesticides.
- Buy from local farmers who use fewer or no synthetic pesticides.
- Incorporate more Clean Fifteen items into your diet.
- Advocate for better food policies by supporting organizations that push for stricter pesticide regulations.
Pesticides pose significant health risks due to their chemical residues, particularly on non-organic produce. While these chemicals may help protect crops, their long-term effects on human health are alarming. By making informed choices, opting for organic alternatives when possible, and pushing for better food safety regulations, we can protect ourselves and future generations from the hidden dangers of pesticides in foods. Your health is in your hands—choose wisely!

by Dr Gene | Apr 12, 2025 | Health
That tattoo you’ve been dreaming of to express your individuality could come with a price.
Tattoos have long been a form of personal expression, cultural identity, and artistic creativity. From ancient civilizations marking their bodies with ink to modern tattoo parlors on every corner, the appeal of permanent body art has never been stronger. For many, getting a tattoo is a deeply personal decision, a way to commemorate a meaningful event, honor a loved one, or simply showcase individuality. Yet, while tattoos have become increasingly mainstream, their potential health risks are often overlooked.
For all their beauty and significance, tattoos involve a process that carries inherent risks, from infections and allergic reactions to long-term complications that science is still working to understand. Despite advances in tattooing technology and improvements in hygiene practices, concerns remain about how tattoo ink interacts with the body over time and what implications it may have for overall health.
At the core of the tattooing process is the injection of ink into the skin using a needle that penetrates the dermis, the second layer of skin. Unlike surface-level cosmetics, which fade or wash away, tattoo ink is deposited deep enough to become permanent. This process requires precision and sterility, but even in the most controlled environments, there are risks associated with piercing the skin barrier. One of the most immediate concerns is infection. The skin acts as a natural shield against bacteria, viruses, and harmful chemicals, and when that protective barrier is breached, the risk of contamination rises. Poorly sanitized needles can introduce dangerous pathogens, leading to bacterial infections, hepatitis, or even HIV if strict hygiene protocols are not followed.
Beyond immediate infections, another major concern is the long-term effects of tattoo ink in the body. Recent research suggests that tattoo ink doesn’t just stay in the skin—it travels. The immune system attempts to clean out the ink particles, which are foreign to the body. Over time, fragments of tattoo pigment migrate to the lymph nodes, where they accumulate. This raises concerns about long-term health effects, particularly related to the lymphatic system and the body’s immune response.
New evidence suggests a potential link between tattoos and cancer, specifically lymphoma, a cancer that begins in the germ-fighting lymphatic system. According to a study from Lund University in Sweden, published in The Lancet’s eClinicalMedicine, individuals with tattoos had a 21 percent higher risk of developing malignant lymphoma compared to those without tattoos. The study analyzed nearly 12,000 people aged 20 to 60 and found that having just one tattoo significantly raised the odds of developing the disease.
Perhaps even more alarming is that the timing of when a person received their first tattoo seemed to influence cancer risk. Those who got their first tattoo less than two years before being diagnosed had an 81 percent higher risk of developing lymphoma. Interestingly, the risk appeared to decrease in those who had gotten tattoos between three and ten years prior, but it rose again for individuals who had their first tattoo eleven or more years ago, showing a 19 percent increased risk.
Size didn’t seem to matter in determining lymphoma risk, which suggests that even a small tattoo could trigger an immune response capable of affecting long-term health. Researchers speculate that low-grade, chronic inflammation caused by tattoos may be a contributing factor in cancer development, though the exact mechanisms remain unclear.
This latest study is not the only research linking tattoos to cancer risks. A study presented at the 2023 American Association for Cancer Research Annual Meeting found a potential connection between having three or more large tattoos and higher risks of blood cancers, myeloid neoplasms (bone marrow cancers), and lymphoma. The study also indicated that individuals who received their first tattoo before age 20 had an elevated risk of developing myeloid neoplasms, while those who got their first tattoo at age 20 or older were more likely to develop lymphoma.
Another concern is the composition of tattoo ink itself. The FDA does not regulate tattoo ink as strictly as other cosmetic or medical products, and many inks contain unlisted substances that could be toxic to human health. A 2022 study published in Toxicology and Industrial Health found that many tattoo inks contain hazardous chemicals, including heavy metals like lead, arsenic, and mercury, which could pose long-term risks to organs, immune function, and overall health. These toxic substances, once inside the body, may contribute to chronic inflammation, cell damage, and potentially cancer development.
Further complicating matters, certain ink colors appear to carry different levels of risk. A 2021 case series linked black and red tattoo inks to an increased risk of melanoma, basal cell carcinoma (the most common type of skin cancer), and dermatofibrosarcoma protuberans, a rare and aggressive soft tissue tumor. Red ink, in particular, has been associated with severe allergic reactions and chronic inflammation.
While the link between tattoos and cancer is still being explored, scientists agree that tattoo ink does not remain harmlessly in the skin. The body’s natural immune defenses constantly try to break down and remove ink particles, sending them to the lymph nodes and other areas of the body. In some cases, this can cause lymph node discoloration and swelling, while in others, it may contribute to long-term health complications that researchers are only beginning to understand.
Aside from cancer risks, tattoos can also cause chronic skin conditions. Some individuals experience allergic reactions to tattoo ink, leading to itching, redness, and long-term inflammation. In extreme cases, granulomas—small, painful lumps caused by an immune reaction—can form around tattoo pigment. Tattoos can also lead to keloid scarring, where the skin overproduces collagen in response to trauma, resulting in raised, thickened scars that can be difficult to remove.
Laser tattoo removal, often sought by individuals who regret their ink, introduces its own set of health concerns. The laser process breaks down pigment into smaller particles, which are then absorbed into the bloodstream and filtered out by the liver and kidneys. Some experts worry that this process could further distribute harmful substances throughout the body, potentially increasing the risk of toxicity or other adverse effects.
While none of this research suggests that every tattoo will lead to cancer or serious illness, it does raise important questions about the long-term safety of tattooing. Scientists acknowledge that more studies are needed to understand the full extent of the risks. But given the growing evidence that tattoo ink interacts with the body in complex and potentially harmful ways, it is clear that individuals considering a tattoo should be fully informed about the possible health implications.
So, what does this mean for those who already have tattoos or are thinking about getting one? While tattoos remain a deeply personal choice, awareness is key. Choosing a reputable tattoo artist who follows strict hygiene protocols reduces the risk of infection. Asking questions about the composition of tattoo inks can also help minimize exposure to harmful chemicals. And, most importantly, people should pay close attention to their health, monitoring for any unusual skin reactions, swelling, or persistent inflammation near tattooed areas. If any concerning symptoms arise, seeking medical advice is essential.
As tattoos continue to be a popular form of self-expression, it’s important to balance their artistic and cultural significance with an understanding of the risks. While tattoos may seem like an aesthetic decision in the moment, the long-term impact on the body is something science is still uncovering. Making an informed choice about body art isn’t about fear—it’s about ensuring that personal expression doesn’t come at the cost of long-term health.

by Dr Gene | Apr 10, 2025 | Health
In today’s society everyone craves a quick fix, and weight loss has become one of the most sought-after goals. People are constantly looking for shortcuts and hacks that promise fast results with minimal effort—whether it’s a miracle pill, an extreme diet, or even surgery. But the reality is that while these shortcuts might lead to short-term weight loss, they rarely translate into long-term success. More importantly, they often fail to promote true health and longevity.
Losing weight isn’t just about shedding pounds; it’s also about enhancing overall well-being, increasing lifespan, and maintaining high energy levels. However, many popular weight loss strategies completely miss the point by neglecting to address the root causes of weight gain. As a result, individuals often find themselves caught in a frustrating cycle of yo-yo dieting, metabolic damage, and ongoing disappointment. This dependence on quick fixes often leads to short-term success, followed by inevitable weight regain, making it increasingly challenging to sustain a healthy body in the long run.
One of the most common approaches to rapid weight loss is extreme caloric restriction, also known as crash dieting. People drastically cut their calorie intake—sometimes to as low as 800 to 1200 calories a day—believing that consuming fewer calories will rapidly melt away body fat. While this may lead to quick results on the scale, the body responds by slowing down metabolism to conserve energy. Instead of burning fat efficiently, the body starts breaking down muscle, ultimately reducing the number of calories burned daily. When normal eating resumes, the metabolism remains sluggish, and the weight returns even more easily. Additionally, extreme caloric restriction can lead to severe nutrient deficiencies, fatigue, hair loss, and hormonal imbalances, making it an unsustainable and harmful approach to weight loss.
Intermittent fasting (IF) and one-meal-a-day (OMAD) diets are other strategies that people use to accelerate fat loss. Both intermittent fasting and caloric restriction are effective methods for weight loss, offering proven health benefits. However, they represent lifestyle changes rather than shortcuts to weight loss. By skipping meals or limiting eating to a narrow time window, individuals attempt to “trick” their bodies into burning more fat. While some people achieve success with this method, others face extreme hunger, energy crashes, and the risk of binge eating once their fasting period concludes. Moreover, if intermittent fasting is not paired with a well-balanced diet, it can lead to muscle loss, nutrient deficiencies, and hormonal imbalances. Many individuals who try fasting ultimately abandon it due to its unsustainable nature, demonstrating that while it may be an effective tool for some, it is far from a one-size-fits-all solution.
The ketogenic diet and other low-carb approaches have surged in popularity due to their promise of rapid fat loss. By eliminating most carbohydrates, the body enters ketosis, a metabolic state in which it burns fat instead of glucose for energy. This approach has merit as a life-style change, and there are numerous documented health benefits, but many people find the diet is incredibly difficult to sustain, as many find it challenging to eliminate carbohydrates long-term. When it comes to short-term weight loss, much of the initial drop in weight comes from water loss rather than fat loss. If not carefully managed, keto can lead to nutrient deficiencies, digestive issues, and unpleasant side effects like the “keto flu,” which includes fatigue, nausea, and irritability. Many people who abandon keto quickly regain the weight once carbohydrates are reintroduced, demonstrating that extreme dietary restrictions rarely provide long-term results.
Other common shortcuts include meal replacement shakes and liquid diets. While replacing meals with shakes or smoothies may seem like an easy way to control calorie intake, these approaches rarely instill sustainable eating habits. Many meal replacement shakes lack the fiber and essential nutrients found in whole foods, leading to increased hunger and cravings. Additionally, severe calorie restriction through liquid diets can slow down metabolism, making long-term weight maintenance even more difficult. Once individuals return to normal eating, the weight often returns just as quickly as it was lost.
Besides dietary shortcuts, many people resort to medications and stimulants to speed up weight loss. Prescription appetite suppressants like Phentermine, along with over-the-counter fat burners, offer a temporary solution by curbing hunger and boosting metabolism. However, once the medication is discontinued, hunger returns strongly, resulting in weight gain. Many of these stimulants have unwelcome side effects, including anxiety, elevated heart rate, and insomnia, rendering them an unsustainable and potentially risky option. While they may provide an initial boost for weight loss, they fail to tackle the underlying behaviors that lead to excess weight in the first place.
Weight loss drugs, such as GLP-1 receptor agonists like Ozempic, Wegovy, and Mounjaro, have gained significant popularity due to their ability to reduce appetite and promote rapid weight loss. While these medications can be effective, they are expensive and require ongoing use to sustain results. Many individuals experience side effects like nausea, fatigue, and even muscle loss, causing some to discontinue the medication. The long-term effects on the body remain unknown. However, the greatest concern is that these drugs do not promote healthy eating habits. Many people tend to regain the weight after stopping the medication, highlighting the importance of making long-term lifestyle changes instead of relying solely on medication.
For those seeking more drastic solutions, bariatric surgery—such as gastric bypass or sleeve gastrectomy—can lead to significant weight loss by physically reducing stomach size and limiting food intake. While bariatric surgery can be life-changing for individuals with severe obesity, it is far from a quick fix. The procedure carries significant risks, including complications, nutrient deficiencies, and long-term digestive issues. Furthermore, if patients do not commit to making permanent lifestyle changes, weight regain is still possible even after surgery.
Some people turn to even more extreme measures like laxatives, detox teas, and diuretics in an attempt to “flush out” weight. These methods do not actually result in fat loss—they simply lead to water loss and dehydration. The reliance on these products can be dangerous, as they disrupt electrolyte balance and may cause digestive problems or dependency. Despite their popularity in marketing and social media, detox teas and cleanses are little more than scams that fail to deliver any meaningful weight loss results.
So, when these shortcuts fail, what truly works for sustainable weight loss and long-term health? The answer lies in sustainable lifestyle changes rather than extreme restrictions or quick fixes. Instead of starving the body, the key is to create a moderate calorie deficit that allows for gradual and maintainable fat loss. Prioritizing protein and whole foods helps preserve muscle mass, control hunger, and support overall metabolic health. Strength training and daily movement ensure that the body remains strong, lean, and capable of burning calories efficiently. Quality sleep and stress management are equally crucial, as poor sleep and chronic stress can increase cravings and contribute to fat storage. Finally, the most important factor in long-term weight management is finding an enjoyable and sustainable approach.—because if a diet or workout routine feels like punishment, it won’t last.
Weight loss should never be about pursuing the quickest possible results. Instead, it should involve transforming into the healthiest version of yourself, one step at a time. Quick fixes may provide temporary relief but ultimately overlook the bigger picture of long-term health and well-being. For genuine and lasting weight loss, concentrate on developing sustainable habits that lead to a longer, stronger, and healthier life. True wellness is not about losing weight rapidly—it’s about maintaining weight loss at a level your individual body requires and thriving for decades to come.
If you’re ready to transform your health the right way, The Longevity Series provides science-backed strategies to help you live longer, healthier, and stronger—without the gimmicks.